Due to the scarcity of tests across the country, hospitals usually only test those cases that they need to admit to the hospital. The hospitals are not testing the majority of people complaining of symptoms, nor the many possibly infected asymptomatic people. We need to keep this fact in mind when looking at the statistics being tracked by Johns Hopkins University, The New York Times, and Worldometers.
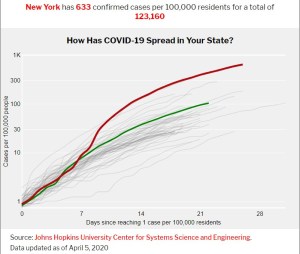
Let us focus on the statistics for New York state, because that is one geographical entity where we know testing only the sick is the policy. This region is the origin of the largest number of cases in the U.S. As of today, April 6, 2020, there are 130,000 cases of COVID19 confirmed in NY state. Those numbers came from about one-third of the 302,000 administered tests that came back positive. It is more interesting to consider these numbers on a per capita basis, to learn how widely the virus is spread in the community. About 1.5% of the population has been tested, and about 0.67% of the population has shown a positive result from the tests.
Now let’s step back and ask the real question: how many infected patients become candidates for admission to the hospital? Only a few places in the world are not being strictly reactive to the crisis and have tested enough people to have a handle on the overall retrospective distribution of outcomes. Reports from the outbreak in China suggest that about 15% to 20% of those infected eventually need hospitalization.
The point is, if we are only testing patients imminently needing hospitalization, then we are missing the other 80 to 85% of the cases that are milder. Since those milder cases are not tested, they are not even counted. If we go back to hard-hit New York and make a correction for the case numbers based on this information, then we can expect that the real case prevalence in the community is likely 5 times higher than what is reported, about 3% of the population; that is to say, one in 30 people are sick.
My concern is that once you reach this level of infection, it becomes very difficult to tamp it back down. There are just too many opportunities for the infection to spread further. I hope I’m wrong on this, and that social distancing will do its job. But if the infection rate continues to run, there are only a few more doublings possible before everyone has it. The reported case rate is still doubling in New York every 6 or 7 days, so one could expect half of the people in the city to have contracted it in four more doublings or about 25 days – by the end of the month. Only then will the infection really run out of steam, because there will be no more virgin immune systems of which to take advantage. Until we have a vaccine, the only thing really fighting this virus are the immune systems of the victims it infects.
In the early days before social distancing, an infected individual would spread the infection to, on average, another 2.4 people. To bring the pandemic under control, that number needs to be reduced to less than one.
There are two possible outcomes for this first round of infection from COVID-19. We could be effective with social distancing and reduce the infection rate to something that is manageable, where individual cases are few enough that communities can trace all contacts and isolate them to prevent further infection. The second option is for the virus to run through the community until it has infected at least half of us. When an infected individual, while still infectious, no longer manages to infect another person (because there just aren’t that many susceptible people to come in contact with anymore), the epidemic will end. By the end of the summer, different parts of the country could have these very different outcomes.
Reference:
Covid-19: four fifths of cases are asymptomatic, China figures indicate

Testing only the severely ill is almost pointless since there are no specific treatments for the virus. At that point in the disease progression the ICU people are simply focused on keeping the patient oxygenated and alive. No testing for those who are displaying a well known array of symptoms, along with no solid plans for isolating those who are positive from family members and others, is a sure fire way to grease the skids for the movement of this virus from person to person. Social distancing can only do so much, those infected have to be identified, removed from contact with others, and treated. None of this is taken place. There is no plan in place. A total sh_tshow.
Michael, I think many hospitals are totally overwhelmed at this point. As you say testing is almost pointless. Less overwhelmed hospitals can at least know who to isolate from who with results of the test – so does have its place. Only tool at the moment is to reduce virus growth rate by limiting contact with others. If that manages to significantly reduce new case numbers to just a handful, then testing and tracing contacts makes sense. So… get used to your living room!
As a relatively healthy and low-risk person living in a place where the virus’ effects on the healthcare system have been minimal, would it be best for society for me to intentionally expose myself to the virus and then immediately self-isolate as a way of developing immunity without infecting others? I don’t know if this is even feasible, but I raise it as a thought experiment.
I’m worried that social distancing measures might be tolerable for a month or two but not long enough for a vaccine to be developed. Perhaps it’s possible for some level of “herd immunity” to be achieved with minimal impact on those who have the highest risk of complications. Of course some small fraction of otherwise healthy people do develop severe symptoms and we’d have to be prepared for that, making sure that the burden on the healthcare system stays manageable.
This seems like a wise course of action if we assume it is inevitable that e.g. 50% of the population will be infected over the next year… this is an arguable position, but not definitively true.
Jon – Intentionally exposing oneself is a gamble at any age. IMHO, what we need is widespread, actually, universal testing, to identify those who have it and keep them from infecting others, especially enough tests for first line medical staff. Second, we need widespread antibody testing. Someone with a negative viral test and positive antibody test should be immune and non-infective, able to return to the workplace. It’s now believed that anywhere from 1/4 to 1/2 of those infected had no symptoms, and these people need to be identified and given some sort of certification so they can return to the workforce (I’m wondering when I’ll be able to get a haircut again, for example). What we need is a coherent, coordinated program to deal with this, and so far all we have is social distancing.
I’ve wondered the same. Sort of a self-vaccination. I think this would work best if there was a way to know how to expose yourself to a very small viral dose. Young healthcare workers have poorer outcomes compared to the same age group in the general public – presumably because they are infected with larger levels of virus when exposed. But this isn’t something anyone is studying at the moment.
The corollary is that the vulnerable population will need to take precautions indefinitely until a vaccine is available. Even after there is general herd immunity, there will be hot spots and a mobile population that will bring in virus from elsewhere. There is not much discussion today about the end game…
Testing be less pointless if this is viable:
https://www.dailywire.com/news/study-coronavirus-treatment-using-blood-plasma-from-recovered-patients-helped-infected-get-better-within-three-days
Sweden is using the approach of not locking down, but rather letting less vulnerable people remain at large. Time will tell whether that was the better approach, I think.